Sent to the patients of My Doctor Medical Group on 4/10/2020 by Paul Abramson MD
To Our Patients,
Keep reading for more information about how to get medical care during this difficult time, how to provide support and two free therapy sessions for first responders/front line medical professionals, and how we are providing medical services while we are sheltering in place.
Answers to the most commonly asked questions about COVID-19:

Paul Abramson MD
Medical Director
Q: What's the status of COVID-19 in San Francisco?
A: “Flattening the curve” seems to be working, so far. ERs and hospitals are not busy and not full as all elective surgery and almost all outpatient activity was cancelled. We’re seeing lower rates of heart attacks, hip fractures, appendicitis, and many other illnesses as fewer people are exposed to risky activity or other diseases.
Q: Should I be afraid of going to the ER for a non-COVID illness?
A: No. Hospitals are not full, resources are plentiful, and access to emergency care is excellent. Dr. Abramson can get you a private room directly at CPMC, St. Francis or St. Mary's on short order. There's no current reason to be afraid of needing hospital care.
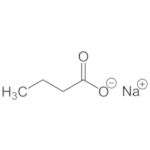
Q: What's up in at My Doctor Medical Group?
A: We’re here. We're all-hands-on-deck working hard to serve our patients. Your options for care are during this time are:
- Online video conference: Speak with any of our doctors and staff through video chat. Over 95% of our patients are pleased with this option.
- Home and hospital visits: Dr. Abramson, Justin Davis, and our affiliated physicians can visit you, as needed, in full PPE to reduce risk of infection.
- Office visits: SIP guidelines allow for visiting doctor’s offices and pharmacies. We have a dedicated safe space at our office for urgent care.
- COVID-19 Testing: Both PCR swabs and antibody testing are available in the office or at your home or workplace. Employer based testing can be arranged for groups, too.
Q: What hospital should I go to if I get sick in or near San Francisco?
A: We recommend one of the hospitals where Dr. Abramson and his team have privileges:
First choice:
Sutter CPMC Van Ness Campus (1101 Van Ness).
Alternatives:
- Sutter CPMC Davies (45 Castro) or Mission Bernal Campus (3555 Cesar Chavez).
- St. Francis Hospital (900 Hyde)
- St Mary's Hospital (450 Stanyan St).
- If necessary: UCSF
First Responder/Health Care Worker Support
Our team is actively working with our patients on stress-related issues. All of these services are available over video chat. We offer:
- Free counseling for front line personnel. We are offering two free video counseling sessions after which continuation in our practice is possible or referral elsewhere. Go to https://mydoctorsf.com/contact to schedule a session.
- “Psychological First Aid” is available for those suffering from acute symptoms and need immediate care and support.
- Psychotherapy: Our three expert psychotherapists are available as always.
- Stress support: Some people are benefitting from (safe) medications and/or dietary supplements for anxiety, sleep, and other stress-related issues. We are very thoughtful in our prescribing.
- Regular check-ins: Regular chats with a doctor who is up-to-date on the current COVID-19 situation and government guidelines can address any new or on-going non-urgent concerns.
I hope this message has been helpful to you. We're in the office M-F 9am-5pm and available for urgent issues 24/7.
- This information is also available for reference and/or sharing at https://homecovidtest.com/blog
- Our practice web site is https://mydoctorsf.com
Sincerely,
Paul Abramson MD
Medical Director, My Doctor Medical Group
Assistant Clinical Professor, UCSF
415-963-4431
[email protected]









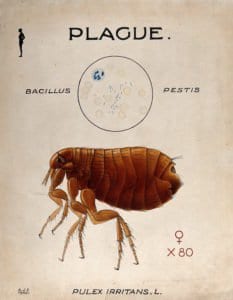
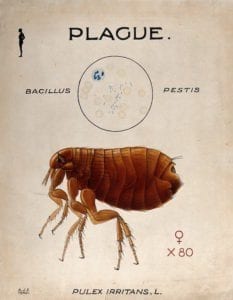 World Health Organization Advisory: Plague in Madagascar: October 2017
World Health Organization Advisory: Plague in Madagascar: October 2017
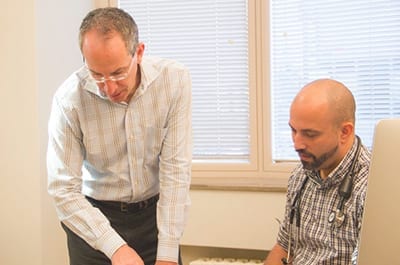
 Dr. Abramson was interviewed on NPR Morning Edition by Amy Standen yesterday about the role of wearable technology and health apps in the doctor's office.
Dr. Abramson was interviewed on NPR Morning Edition by Amy Standen yesterday about the role of wearable technology and health apps in the doctor's office.
 Giardiasis is a fairly common infection of the small intestines caused by the organism Giardia intestinalis (also known as Giardia lamblia). Giardia is a protozoan parasite that thrives in the intestinal tract of mammals and that reproduces by forming cysts, which are transmitted from host to host through the feces of an infected person or animal being ingested by another. The cysts are very resistant and can survive for long periods of time in fresh water, such as lakes, streams and reservoirs.
Giardiasis is a fairly common infection of the small intestines caused by the organism Giardia intestinalis (also known as Giardia lamblia). Giardia is a protozoan parasite that thrives in the intestinal tract of mammals and that reproduces by forming cysts, which are transmitted from host to host through the feces of an infected person or animal being ingested by another. The cysts are very resistant and can survive for long periods of time in fresh water, such as lakes, streams and reservoirs.


 This past Thursday, Dr. Abramson and I attended the Quantified Self Conference in the Presidio in San Francisco. We hosted a morning breakout session titled “Quant-Friendly Doctors and Doctor-Friendly Quants” that drew a very passionate and diverse crowd. We began by describing what exactly it is we are doing in our medical practice with self-tracking and our unique Quant Coaching Program. The questions and debates sparked were interesting and at times emotionally charged. Little did we know that one astute woman in the audience was live tweeting the whole thing!
This past Thursday, Dr. Abramson and I attended the Quantified Self Conference in the Presidio in San Francisco. We hosted a morning breakout session titled “Quant-Friendly Doctors and Doctor-Friendly Quants” that drew a very passionate and diverse crowd. We began by describing what exactly it is we are doing in our medical practice with self-tracking and our unique Quant Coaching Program. The questions and debates sparked were interesting and at times emotionally charged. Little did we know that one astute woman in the audience was live tweeting the whole thing!
 My Doctor Medical Group founder Paul Abramson MD was interviewed this week in the San Francisco Chronicle about his use of self tracking technologies, in collaboration with “Quant Coach” Lauren DeDecker, to collaboratively help his patients in San Francisco solve vexing health challenges, taking the do-it-yourself Quantified Self approach to a professionally-supervised level.
My Doctor Medical Group founder Paul Abramson MD was interviewed this week in the San Francisco Chronicle about his use of self tracking technologies, in collaboration with “Quant Coach” Lauren DeDecker, to collaboratively help his patients in San Francisco solve vexing health challenges, taking the do-it-yourself Quantified Self approach to a professionally-supervised level.
 Truer words have not been spoken, by Dr. Arnold Wald in a recent
Truer words have not been spoken, by Dr. Arnold Wald in a recent