Can psychedelics ease the suffering of those with terminal illness? A growing number of medical studies, and a recent article in the New York Times, say “yes.”
Can psychedelics ease the suffering of those with terminal illness? A growing number of medical studies, and a recent article in the New York Times, say “yes.”
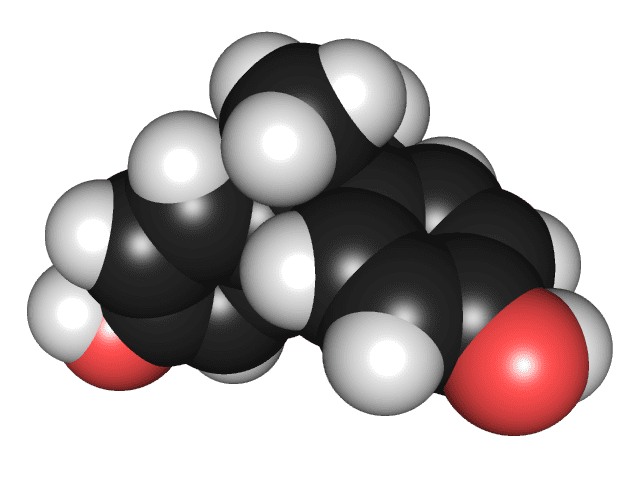
Research into the use of psychedelic and entheogenic drugs, such as psilocybin-containing mushrooms, LSD and MDMA, to treat medical and psychiatric problems was actively pursued in the 1950s and 1960s. Recently, after a decades-long hiatus due to government reaction to cultural factors in the 1960s, research has begun again. The initial focus has been on mental health issues such as anxiety in terminally-ill patients and PTSD in military veterans. But using these substances to treat medical conditions, such as LSD for cluster headaches, has also shown promise.
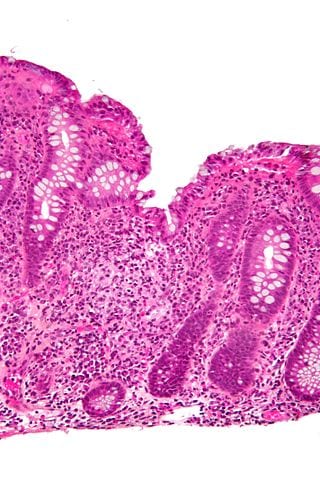
Pam Sakuda was 55 when she found out she was dying. Shortly after having a tumor removed from her colon, she heard the doctor’s dreaded words: Stage 4; metastatic. Sakuda was given 6 to 14 months to live. Determined to slow her disease’s insidious course, she ran several miles every day, even during her grueling treatment regimens. By nature upbeat, articulate and dignified, Sakuda — who died in November 2006, outlasting everyone’s expectations by living for four years — was alarmed when anxiety and depression came to claim her after she passed the 14-month mark, her days darkening as she grew closer to her biological demise. […]
Norbert Litzinger remembers picking up his wife from the medical center after her first [psychedelic] session and seeing that this deeply distressed woman was now “glowing from the inside out.” […] under the influence of the psilocybin, she came to a very visceral understanding that there was a present, a now, and that it was hers to have.
The latest study out of UCLA, published in the Archives of General Psychiatry in 2011 and conducted by Charles Grob MD, administered psilocybin — an active component of magic mushrooms — to end-stage cancer patients to see if it could reduce their fear of death.
The results showed that administering psilocybin to terminally ill subjects could be done safely while reducing the subjects’ anxiety and depression about their impending deaths.
Surely more research is needed. And these drugs are currently all still in Schedule 2 of the Controlled Substances Act in the United States. So any use outside of a DEA-approved research protocol is illegal.
You can find the entire NYT article here.